Question 23M.2.HL.TZ2.1
| Date | May 2023 | Marks available | [Maximum mark: 14] | Reference code | 23M.2.HL.TZ2.1 |
| Level | HL | Paper | 2 | Time zone | TZ2 |
| Command term | Calculate, Deduce, Identify, Outline, Predict, Suggest | Question number | 1 | Adapted from | N/A |
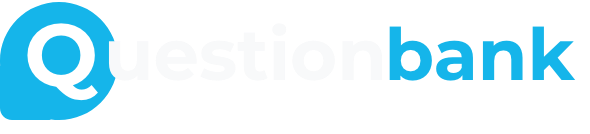
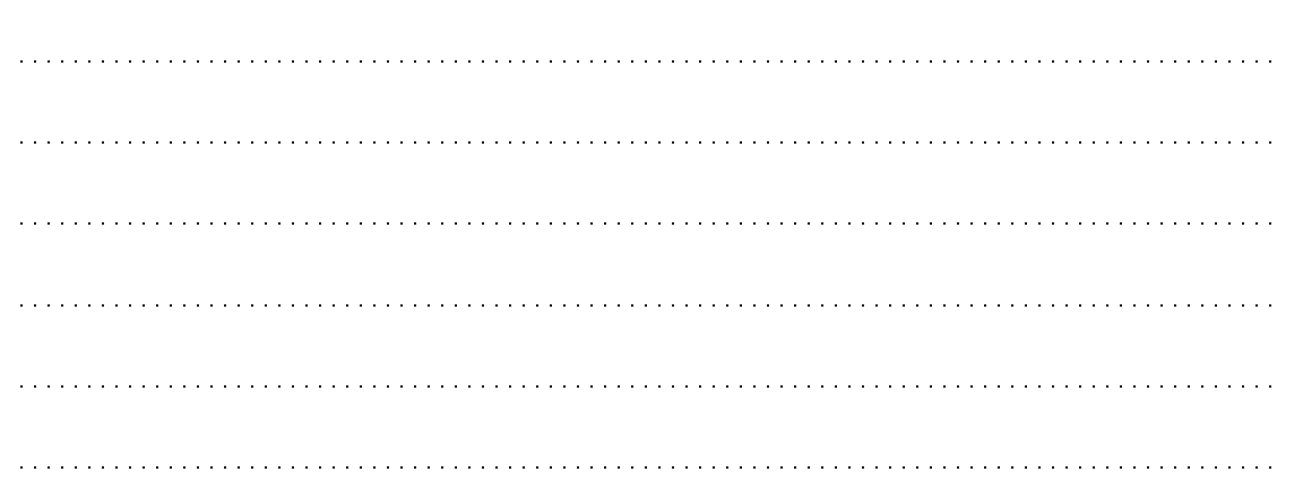
Vaccination programmes have led to decreases in child mortality. The graph shows global trends between 1980 and 2018 in the vaccination of children against seven different pathogens in the first year of their lives.
[Source: Adapted from World Health Organization and UNICEF, 2019. Global vaccination coverage, world, 1980 to 2018.
[graph online] Available at: https://ourworldindata.org/grapher/global-vaccination-coverage?time=earliest..2018&country=~OW
ID_WRL [Accessed 8 October 2021]. Public domain.]
Using the graph, identify the percentage who had received the tuberculosis vaccine in 2012.
[1]
89%;
Allow 88 to 91 %.
Calculate the difference in time between 40 % of children receiving the hepatitis B vaccine and 40 % receiving the pneumococcal vaccine.
[1]
13 years;
Allow any value between 13 and 14 years inclusive.
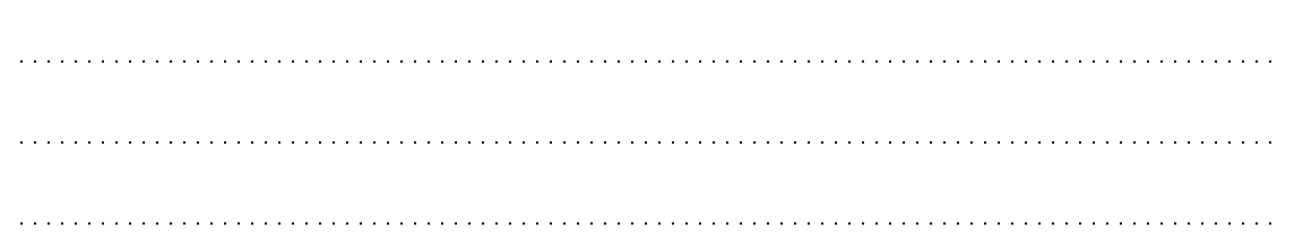
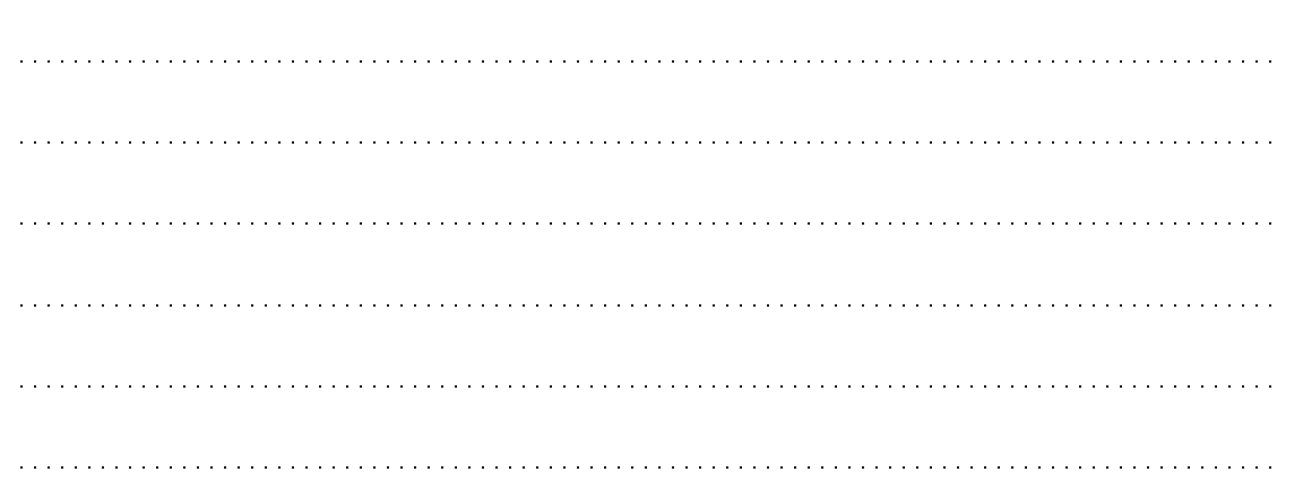
Children are immunized against diseases caused by Streptococcus pneumoniae with pneumococcal conjugate vaccine (PCV) and against diseases caused by Haemophilus influenzae with Haemophilus influenzae type b (Hib) vaccine.
The graphs show the estimated global percentages of children not vaccinated against S. pneumoniae and H. influenzae by the age of 5 and the estimated global death rates in children under 5 years, due to these pathogens, between 2000 and 2015.
[Source: Adapted from Wahl et al., 2018, Burden of Streptococcus pneumoniae and Haemophilus influenzae type b disease in children in the era of conjugate vaccines: global, regional, and national estimates for 2000–15. The Lancet Global Health 6 (7), E744-757. https://www.thelancet.com/journals/langlo/article/PIIS2214-109X(18)30247-X/fulltext. Open access.]
Outline the conclusions that can be drawn from the graph showing data for PCV and S. pneumoniae.
[2]
- number of deaths (due to S. pneumoniae) and percentage of children not vaccinated (with PCV) both fall (along the years)
OR
number of deaths (due to S. pneumoniae) decreases while percentage of vaccinated children (with PCV) increases (along the years); -
positive correlation between number of deaths and percentage of children not vaccinated /
OR
negative correlation between number of deaths and percentage of children vaccinated / vaccination reduces the number of deaths; - increased reduction in the number of deaths from 2010 onwards;
- still large number of deaths/large number of children unvaccinated in 2015;
Comparative terms expected (do not award mp for just stating values).
Mpb: do not allow “directly or inversely proportional”.
Mpb: Do not just accept “positive correlation” or “negative correlation” without a clear indication of the variables being correlated
Suggest reasons for the difference between the data for S. pneumoniae and H. influenzae.
[2]
- Hib vaccination program started earlier/PCV vaccination program started later
OR
Hib vaccine developed before PCV vaccine; - deaths due to H. influenzae drop earlier than deaths due to S. pneumoniae because of earlier vaccination;
- more deaths due to S. pneumoniae than H. influenzae (in any year) as lower % of children vaccinated against S. pneumoniae (compared H. influenzae);
Mp a to c: accept vice versa.
Comparative terms expected (do not award mp for just stating values).
Mpa and mpb: there must be a clear reference to time.
Mpc: there must be clear indication to vaccination.
Allow no points for bacterial virulence / disease severity, etc., as bacterial pathogenicity is not addressed on graphs.
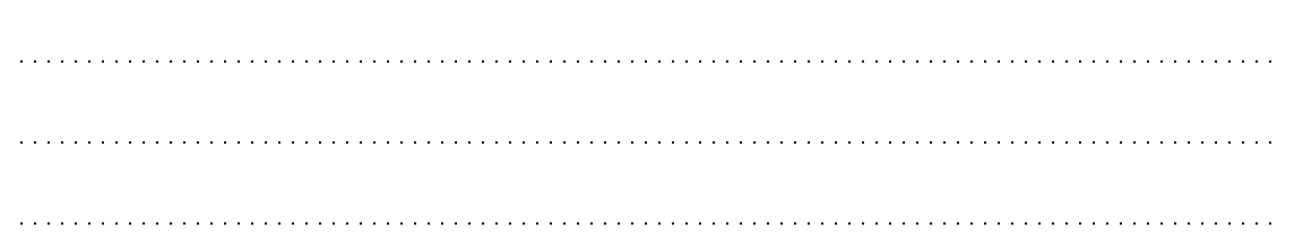
Acute respiratory infection (ARI) is a frequent reason for antibiotic use among children in low-income and middle-income countries (LMICs). S. pneumoniae is the predominant, but not the only, cause of ARI in children.
In a large-scale study, data were collected in 18 LMICs from 65 815 children under the age of 5. The data were analysed to estimate the fraction of ARI cases among the children that could be attributed to S. pneumoniae as shown in the graphs.
The upper estimate in the graphs is for all cases, whether or not they were treated with antibiotics. The lower estimate is for the subset of cases that required antibiotic treatment. The range of estimates is shown by violin plots, with a point for the median estimate and lines for 95 % confidence intervals.
[Source: Adapted from Lewnard, J.A., Lo, N.C., Arinaminpathy, N. et al., 2020. Childhood vaccines
and antibiotic use in low- and middle-income countries. Nature 581, pp. 94–99.
https://doi.org/10.1038/s41586-020-2238-4. Open access.]
Using the data in the violin plots, deduce the age range at which children are most likely to develop ARI due to S. pneumoniae.
[2]
- 2 – 5 years;
- higher number/value/percentage/attributable fraction for 2 – 5 years (than 0 – 5years);
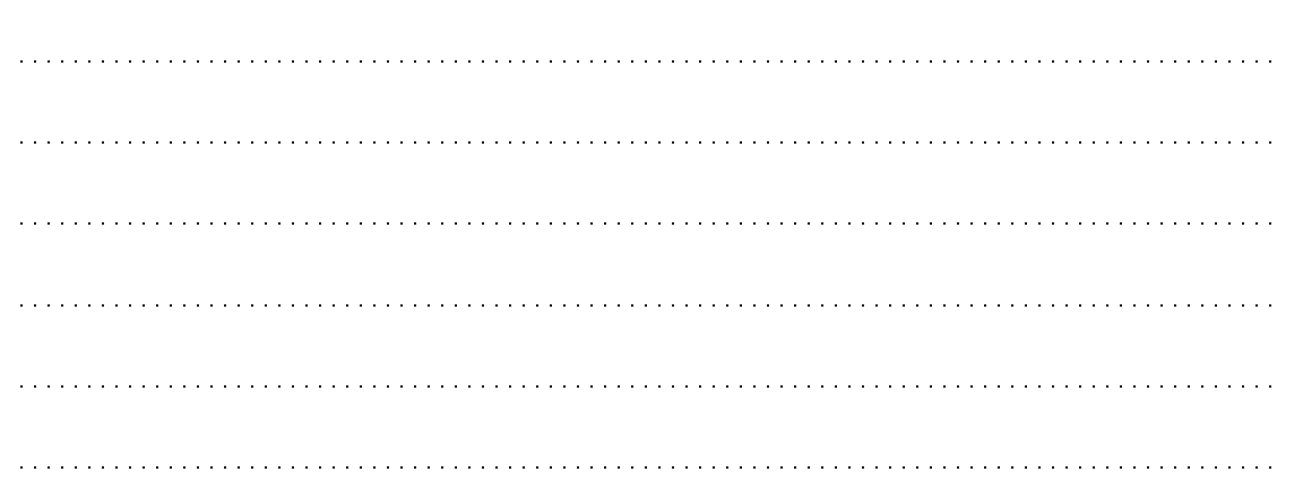
Suggest reasons for the difference between the fraction attributed to S. pneumoniae in all cases of ARI and in cases where antibiotics were used to treat the infection.
[2]
- highest attributed fraction (in both age groups) is in cases where antibiotic used;
- ARI cases due to S. pneumoniae can be severe so antibiotics are often prescribed;
- all cases include other causes / viral ARI which may not require antibiotics;
- antibiotics administered without prescription or physician consultation/to reduce symptoms;
Mpa: Comparative terms expected (do not award mp for just stating values).
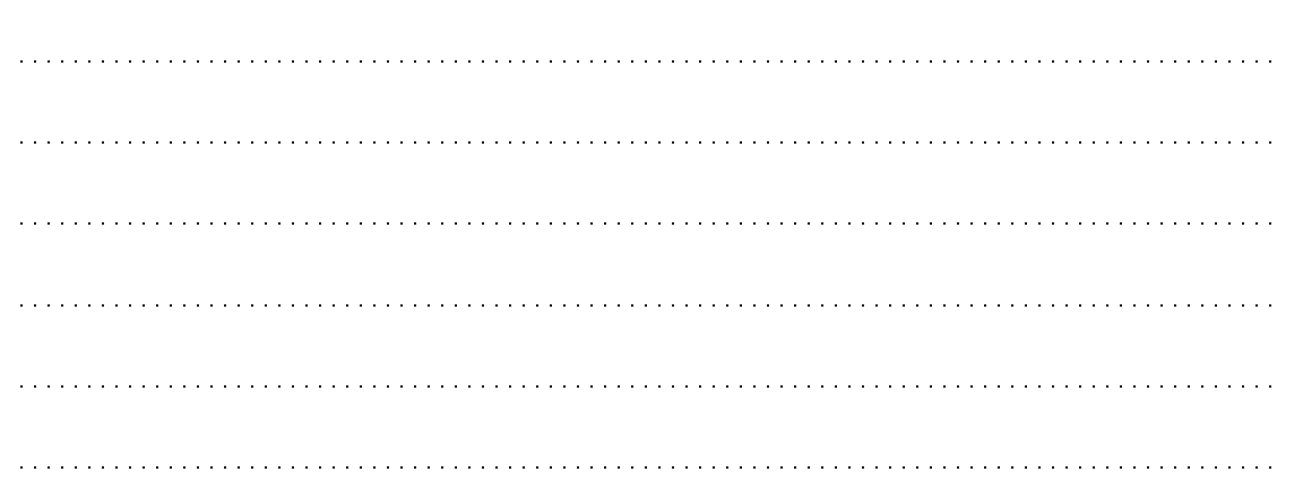
Estimates were made of the extent of antibiotic use in low-income and middle-income countries. Graphs were constructed to show global estimates for the numbers of cases in LMICs per year of ARI treated with antibiotic in children under the age of 5. The estimates for LMICs were divided according to income: low income, lower-middle income and upper-middle income.
The graph shows estimates for three levels of vaccination for S. pneumoniae with PCV:
- no vaccination
- 2018 coverage: the vaccine coverage that there was in 2018
- universal coverage: predictions assuming that in the future all children in all LMICs receive the vaccination.
[Source: Adapted from Lewnard, J.A., Lo, N.C., Arinaminpathy, N. et al., 2020.
Childhood vaccines and antibiotic use in low- and middle-income countries.
Nature 581, pp. 94–99. https://doi.org/10.1038/s41586-020-2238-4. Open access.]
When there is no vaccination, the estimated number of cases for lower-middle income countries is larger than in either low income or upper-middle income countries. Suggest one reason for this.
[1]
- higher population in lower-middle income countries/subgroup (compared to the other 2 subgroups);
- low income population may not have/have less access to medicine/antibiotics/vaccination (compared to lower-middle income population)/ low-income populations may not report data
OR
upper-middle population may have better living conditions/more adequate medical diagnoses (compared to lower-middle income population);
Lower-middle income subgroup is not the same as LMIC (includes all 3 subgroups). LMIC should not be used as equivalent.
Mpb: accept vice versa.
Using the data, predict the effect of universal PCV vaccination in LMICs.
[1]
(worldwide) drastic/huge/important/significant decrease/decrease of 42 million ARI cases (treated with antibiotics);
There must be an indication of magnitude of decrease in the answer for the mark to be awarded.
Accept 30 to 50 million for the decrease.
Outline likely health benefits of universal PCV vaccination of children, other than reducing the incidence of ARI.
[2]
- less use of antibiotics;
- less antibiotic resistance (in pathogens) / antibiotics more successful at treating infectious/bacterial diseases;
- decrease in health care costs / less money spent on antibiotics;
- decreased mortality / protection of immune-deficient patients/non-vaccinated population/ achieve herd immunity;
Since the question already states “other than reducing the incidence of ARI”, this reason should not be accepted.